A psychosocial assessment is a process for learning about a client’s problems and needs, so that together you can create therapy goals and a plan for recovery. The information-gathering process should allow you to learn more about the client as a person, beyond just a diagnosis.
Our Psychosocial Assessment provides an outline for gathering a wide range of information about your client. The assessment includes broad categories to explore, along with reminders for important information.
- Page 1: Demographics and emergency contact information. This can be completed independently by the client, or together in session.
- Page 2: Presenting problem, or the client’s self-reported reason for seeking therapy.
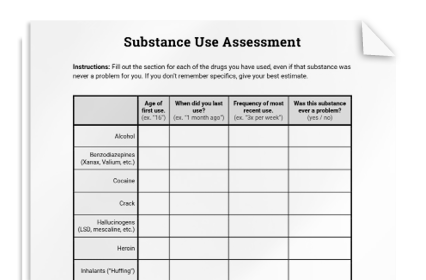
- Pages 3-5: Personal factors, relationships, social and environmental factors, psychiatric factors, family history, physical health, substance use, risk assessment, and strengths and abilities.
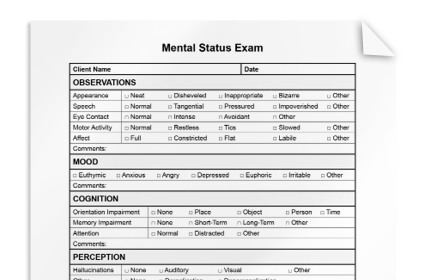
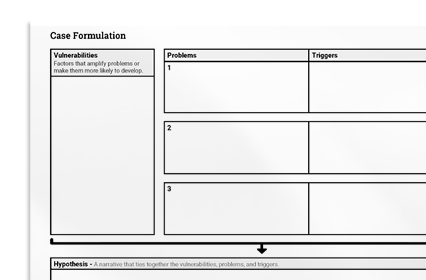
- Page 6: Mental status information and diagnosis, including predisposing, precipitating, perpetuating, and protective factors.
In some cases, you may need to explore a specific area in more depth. When needed, include targeted assessments, such as the substance use assessment, or the mental status exam.
Be mindful of the client’s culture, and how this might impact their experiences, at every stage of the assessment.