Self-harm is a serious mental health concern for teens and adults. As a mental health practitioner, you may be the first to learn that a person is self-harming.
Individuals between the ages of 15 and 24 are the most likely to self-harm. It is estimated that 5% of adolescents engage in serious or frequent self-harm, and 1-4% of adults report some form of self-harm. Despite these statistics, many clinicians don’t regularly assess for this issue.
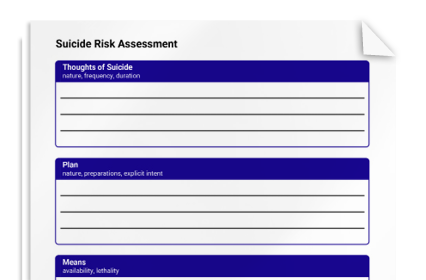
The Self-Harm Assessment is a tool for gathering information about a client’s thoughts, behaviors, and intentions related to self-harm. The categories of questions are as follows:
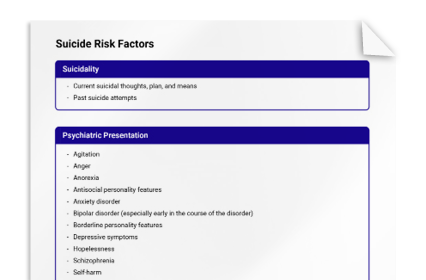
- Suicidal ideation. Even though self-harm isn’t usually about suicide, some people think about suicide when they self-harm. Research has shown that using self-harm as way to avoid suicide is actually one of the strongest risk factors for attempting suicide, and a history of self-harm is a predictor of future attempts.
- Onset, frequency, and methods. Gather information about a client’s first and most recent self-harm behaviors, as well as frequency and methods (e.g., cutting, biting, etc.).
- Aftercare. Learn whether/how the client cares for their self-harm wounds.
- Reasons. Clients may self-harm to try to relieve stress, punish themselves, counteract feeling numb, and more.
- Stage of change. Learn about your client’s motivation to change or stop their self-harm.
This assessment can provide information on the next treatment steps. Common treatment approaches for addressing self-harm include the following:
- Motivational interviewing (MI)
- Cognitive behavior therapy (CBT)
- Dialectical behavior therapy (DBT)
- Emotion-regulation group therapy
As with other issues, self-injury should be met with empathy, and without judgment, to encourage your client to be honest, forthcoming with information, and help-seeking.